Mold is a pervasive problem in many homes, especially in areas with high humidity or poor ventilation. While most people are familiar with the respiratory issues mold can cause, fewer are aware of the potential connection between mold exposure and skin infections, such as staph infections. Staphylococcus bacteria, which can lead to serious health conditions, thrive in damp environments where mold often grows.
In this guide, we’ll explore whether mold can contribute to staph infections, how they might be linked, and steps you can take to protect yourself from both mold-related health risks and bacterial infections.
But before we move into this, let us first take a closer look at what mold is and how it affects our health.
Understanding Mold and How it Affect Our Health
Mold is a type of fungus that thrives in damp, warm, and humid environments. It grows on a wide range of surfaces, such as wood, drywall, carpets, and food. Mold reproduces by releasing tiny spores, which are invisible to the naked eye and spread easily through the air. These spores can land on any moist surface, where they begin to grow and multiply, creating a cycle of contamination. Mold can develop quickly, often within 24 to 48 hours after exposure to moisture, especially in areas with poor ventilation or water damage.
Recommended: Can Kegels Help With Hemorrhoids?
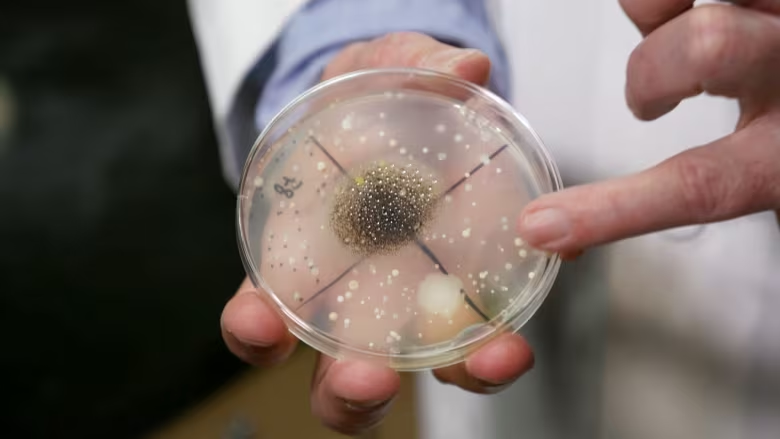
There are thousands of different types of mold, but the most common ones found indoors include Aspergillus, Penicillium, and Cladosporium. Some types of mold are harmless, while others can produce mycotoxins, which are toxic substances that can cause health problems. Mold is typically associated with damp environments, such as bathrooms, kitchens, basements, and areas affected by leaks or flooding.

Mold can cause a variety of health issues, especially for people who are sensitive to it or have existing respiratory conditions. Symptoms of mold exposure may include sneezing, coughing, skin irritation, and respiratory problems like asthma. In more serious cases, mold exposure can lead to chronic health issues, particularly in vulnerable individuals like children, the elderly, and those with weakened immune systems.
What is Staph Infection?
Staph infections, caused by Staphylococcus bacteria, are commonly found on the skin and inside the noses of healthy individuals. Although these bacteria are typically harmless, they can lead to infections if they enter the body through cuts, wounds, or other openings. These infections can range from minor skin issues to severe, potentially life-threatening conditions, depending on the site of the infection and the individual’s health status.

Mild staph infections often appear as boils, cellulitis, or abscesses, characterized by symptoms such as redness, swelling, pain, and pus at the infection site. In more serious cases, staph bacteria can cause conditions like bloodstream infections (septicemia), bone infections (osteomyelitis), or heart infections (endocarditis), all of which demand urgent medical care. Symptoms of these severe infections may include fever, chills, fatigue, rapid heartbeat, or organ dysfunction.
Several factors can increase the risk of developing a staph infection. These include a weakened immune system, chronic illnesses such as diabetes or eczema, extended hospital stays, and living in crowded environments. Staph bacteria can also spread through contaminated food, leading to food poisoning, or through invasive devices like catheters.
The treatment for staph infections depends on their severity. Mild cases are usually treated with antibiotics, while abscesses may require drainage. Severe infections often necessitate intravenous antibiotics or hospitalization to prevent serious complications, such as sepsis, organ damage, or even death.
Preventing staph infections relies on maintaining good hygiene practices. Regular handwashing, keeping wounds clean and covered, avoiding the sharing of personal items, and ensuring proper food storage and preparation are effective measures to reduce the risk. Prompt diagnosis and early medical intervention are crucial for avoiding complications and achieving a faster recovery.
Effect of Mold on the Immune System
Mold exposure can significantly impair the immune system, especially with prolonged or high-level exposure to toxic molds. The immune system serves as the body’s primary defense and mold intrusion can trigger inflammatory responses that disrupt its proper functioning. Here’s a detailed explanation of how mold compromises immunity:
Over-activation of the Immune System
When mold spores are inhaled, ingested, or come into contact with the skin, the immune system identifies them as harmful invaders, initiating a defensive response. This triggers the release of histamines and inflammatory cytokines. In people with sensitivities, such as those with asthma or allergies, this response may become chronic. Over time, this persistent activation can overwork the immune system, reducing its effectiveness against other threats like viruses or bacteria.
Recommended: 3 Human Hormones Most Directly Involved in Sexual Reproduction
Toxic Effects of Mycotoxins
Certain molds, including Aspergillus and Stachybotrys chartarum (black mold), produce harmful substances called mycotoxins. These toxins can enter the body through inhalation, skin contact, or contaminated food. Mycotoxins are known to directly damage immune cells, diminishing their ability to combat infections. Extended exposure to these toxins can lead to immune suppression, leaving the body susceptible to other infections.
Respiratory System Impairment
The respiratory system is a primary entry point for mold spores. Chronic exposure can lead to respiratory conditions like asthma, bronchitis, or allergic rhinitis. Inflammation or weakening of the respiratory system creates a favorable environment for other pathogens, such as Staphylococcus aureus (staph), to thrive. The immune system must then expend extra resources to manage these secondary infections, further straining its capacity.

Chronic Inflammation
Mold exposure often results in chronic inflammation, particularly in individuals with allergies or conditions like Chronic Inflammatory Response Syndrome (CIRS). Prolonged inflammation diverts the immune system’s focus, weakening its ability to address other threats. Over time, this persistent state can impair the body’s capacity to fight routine infections such as colds or flu.
Gut Health Disruption
The gut plays a crucial role in immune function, as it houses a large portion of the body’s immune cells. Mycotoxins from mold can disrupt the gut microbiome by reducing beneficial bacteria and promoting harmful pathogens. This imbalance weakens the gut’s ability to support immune responses, further compromising overall immunity.
Heightened Risks for Vulnerable Groups
Mold exposure poses an even greater threat to individuals with pre-existing health conditions, such as asthma, autoimmune diseases, or allergies. People with compromised immune systems due to conditions like HIV/AIDS, chemotherapy, or diabetes, as well as children and the elderly, are especially susceptible to mold-induced immune dysfunction. For these populations, mold exposure can exacerbate existing health problems and increase vulnerability to infections.
Direct Immune Cell Damage
Mycotoxins and mold metabolites can directly harm immune cells, including macrophages and lymphocytes, which are essential for detecting and eliminating harmful pathogens. When these cells are damaged, the immune system’s efficiency declines, making the body more vulnerable to recurring infections and diseases.
Recommended: 10 Best Vitamins For Hormonal Acne
Long-Term Consequences of Mold Exposure
Prolonged exposure to mould can lead to serious, lasting effects, including:
Autoimmune Disorders
Chronic mould exposure may trigger or worsen autoimmune diseases by causing the immune system to attack healthy tissues due to extended inflammation.
Increased Infection Risk
A weakened immune system becomes more prone to frequent and recurring infections, such as those caused by bacteria like staph.
Delayed Recovery
Mold-exposed individuals often experience slower healing times for injuries and illnesses due to compromised immune efficiency.
How Mold Can Create a Breeding Ground for Staph Bacteria
Mold, a type of fungus, thrives in damp, warm, and poorly ventilated environments. These conditions not only support mold growth but also create a suitable habitat for other harmful microorganisms, such as Staphylococcus bacteria, to flourish. Here’s a closer look at how mold contributes to a breeding ground for staph bacteria:
Moist and Humid Environments
Mold grows in areas with high humidity and moisture, such as bathrooms, kitchens, basements, or water-damaged buildings. These damp conditions also favor the survival and proliferation of Staphylococcus bacteria. Moist surfaces allow bacteria to adhere more easily, creating a stable environment for their growth.
Compromised Indoor Air Quality
Mold releases spores and volatile organic compounds (VOCs) into the air, which can irritate the respiratory system and weaken the body’s defenses. Poor air quality can also make it easier for bacteria, including Staphylococcus, to thrive and spread within a household or building, especially if ventilation is inadequate.

Damage to Skin Barriers
Exposure to mold can irritate or damage the skin, weakening its natural barrier against infections. This makes individuals more susceptible to staph infections, as Staphylococcus bacteria can easily enter through cuts, abrasions, or rashes caused by mold exposure.
Recommended: 10 Best Vitamins For Hormonal Acne
Weakened Immune Response
Chronic exposure to mould and its toxins can weaken the immune system over time, making it less effective at fighting off infections. A compromised immune system increases the risk of staph bacteria taking hold and causing infections, even with minor breaches in the skin or mucous membranes.
Biofilm Formation
Mold and bacteria, including Staphylococcus, often coexist in shared environments. Mold provides an ideal surface for biofilm formation, where bacteria form protective layers that shield them from the immune system and antibiotics. In these biofilms, staph bacteria can grow more resistant and persistent.
Mold-Related Skin Conditions
Mold exposure can lead to skin conditions such as dermatitis or fungal infections, which create opportunities for secondary bacterial infections. Staph bacteria can infect areas already compromised by mold-induced skin issues, worsening the severity of the condition.
Cross-Contamination
Mold and Staphylococcus bacteria can coexist on shared surfaces like damp towels, shower curtains, or kitchen sponges. These items, if not properly cleaned and dried, can act as reservoirs for both mold spores and bacteria, increasing the likelihood of infections in individuals with repeated exposure.
Symptoms of Staph Infection in Mold-Exposed Environments
Mold exposure can weaken the immune system and damage skin barriers, making it easier for Staphylococcus bacteria, which are commonly found on the skin and in the nasal passages, to cause infections. When exposed to mold, the body’s defense mechanisms are compromised, increasing the risk of staph infections in various parts of the body. The severity of symptoms can vary based on the location of the infection and the individual’s health condition.
1. Skin and Soft Tissue Infections
- Boils or Abscesses: These are painful, red lumps filled with pus that are warm to the touch. They typically form when bacteria enter through broken or irritated skin. Mold exposure can increase the likelihood of skin damage, making it easier for staph bacteria to cause these infections.
- Cellulitis: This condition is marked by red, swollen, and tender skin, and it can spread quickly. It occurs when staph bacteria infect the deeper layers of skin and surrounding tissues. The skin may feel warm and painful, and untreated cellulitis can lead to complications.
- Impetigo: This is a skin infection that leads to honey-colored crusted sores, especially on the face and limbs. It is more common in children but can occur in adults as well. The sores can break open, and if left untreated, they can spread the infection.
- Rashes: Mold exposure can cause skin irritation that may resemble an allergic reaction. If staph bacteria infect the irritated areas, they can lead to more severe rashes that require medical attention to prevent complications.
Recommended: Is K Lube Vagina Safe?
2. Respiratory Symptoms:
- Cough: A persistent cough, sometimes with sputum (mucus), is a common symptom of a respiratory staph infection. It occurs when staph bacteria invade the airways, which can irritate the lungs and cause inflammation.
- Fever and Chills: A fever is often a sign that the body is fighting an infection, and chills can occur as the body tries to regulate its temperature. These symptoms indicate a systemic infection that can affect multiple body systems.
- Shortness of Breath: Difficulty breathing may occur if the infection spreads into the lungs. This can make even light physical activity feel exhausting and can worsen as the infection progresses.
3. Foodborne Staph Infections:
- Nausea and Vomiting: These gastrointestinal symptoms are common in foodborne staph infections, where the bacteria contaminate food and enter the body. The body tries to expel the toxins or bacteria by inducing vomiting.
- Diarrhea: Along with nausea and vomiting, diarrhea is a common symptom, as the body attempts to remove the bacteria from the gastrointestinal tract.
- Severe Abdominal Pain: Abdominal discomfort is often associated with foodborne staph infections, caused by inflammation in the stomach or intestines.
- Dehydration: Due to fluid loss from vomiting and diarrhea, dehydration can occur. Symptoms of dehydration include dry mouth, dizziness, and reduced urine output.
4. Bloodstream Infections (Septicemia)
- High Fever: A high fever indicates that the infection has spread into the bloodstream, and the body is mounting an immune response to fight it.
- Rapid Heart Rate: As the infection spreads, the heart may beat faster to circulate blood more quickly in an attempt to deliver oxygen and nutrients to the body’s tissues.
- Low Blood Pressure: In septicemia, the bacteria in the bloodstream can cause the blood vessels to dilate, leading to low blood pressure. This can result in dizziness or fainting.
- Chills and Shaking: These are common when the body is battling a severe infection. The shaking or chills occur as the body tries to regulate its temperature.
- Organ Dysfunction: If the infection progresses, it can cause dysfunction in organs such as the kidneys, heart, and brain. Symptoms may include confusion, reduced urine output, or difficulty breathing.
5. Bone and Joint Infections:

- Deep Bone Pain: If the staph infection spreads to bones, it can cause intense, localized pain that is difficult to relieve. This pain is usually deep in the affected bone.
- Swelling and Redness Over Joints: Joint infections can cause swelling and redness around the affected area, making movement painful and difficult.
- Limited Mobility: The infection may impair movement due to pain and swelling in the affected joint or bone.
- Fever: A persistent fever may accompany bone and joint infections, indicating the presence of a serious infection that needs prompt treatment.
Recommended: Does Vinegar Tighten Your Vagina?
6. Endocarditis (Heart Infection)
- Shortness of Breath: This can occur due to the heart’s reduced ability to pump blood effectively, leading to inadequate oxygen delivery to the body.
- Fatigue: This is a common symptom of a heart infection. Individuals with endocarditis often feel tired and weak, even with minimal physical activity.
- Heart Murmurs: Endocarditis can cause abnormal heart sounds, which may be detected by a doctor through a stethoscope.
- Swelling in the Feet or Legs: This occurs due to fluid buildup from poor blood circulation caused by the infection.
- Persistent Fever: Fever is a common sign of infection, especially when the heart is involved.
7. Toxic Shock Syndrome (TSS):
- High Fever: TSS often presents with a sudden high fever, signaling a severe bacterial infection.
- Widespread Rash: The rash associated with TSS is often red and may spread rapidly across the body.
- Low Blood Pressure: This can cause dizziness and may lead to shock, a medical emergency.
- Vomiting and Diarrhea: These symptoms are often present in TSS, as the body attempts to expel the toxins causing the infection.
- Muscle Pain or Weakness: A generalized feeling of weakness or pain in the muscles is a common symptom of TSS.
- Confusion or Seizures: If left untreated, TSS can lead to confusion, seizures, or loss of consciousness, as toxins affect the brain.
Preventing Mold Growth to Reduce Infection Risk
Mold growth can be minimized through proactive environmental management. By addressing moisture issues, improving ventilation, and maintaining cleanliness, you can significantly reduce the risk of infections associated with mold exposure.
Prevention Methods:
- Control Humidity: Keep indoor humidity levels below 50% using dehumidifiers and air conditioning.
- Fix Moisture Problems: Repair leaks, condensation, and water damage promptly.
- Dry Wet Areas: Clean up spills, dry wet clothes, and eliminate standing water immediately.
- Improve Ventilation: Use exhaust fans in kitchens and bathrooms, and ensure cross-ventilation in living spaces.
- Use Mold-Resistant Materials: Opt for mold-resistant paints, drywall, and insulation during construction or renovations.
- Clean Regularly: Use mould-killing products for routine cleaning of susceptible areas.
- Remove Contaminated Items: Dispose of items with extensive mould growth that cannot be cleaned effectively.
- Proper Storage: Store belongings in waterproof, sealed containers.
- Maintain Outdoor Areas: Clear debris and ensure proper drainage to prevent water accumulation near the home.
- Monitor Conditions: Regularly check for signs of mould or moisture and address issues quickly.
Conclusion
Mold exposure poses significant health risks, including creating a conducive environment for staph infections. Individuals can take proactive steps to minimize exposure and its associated risks by understanding the link between mold and these infections. Preventive measures such as maintaining proper humidity levels, ensuring adequate ventilation, addressing moisture problems, and using mold-resistant materials are essential for fostering a healthier living environment. Timely recognition of symptoms and medical intervention further enhance the ability to manage and mitigate health complications. By prioritizing mold prevention and awareness, we can safeguard both personal health and the structural integrity of our surroundings.